A vulnerable demographic
Patients with issues processing sensory input may have adverse reactions to EEG connection and monitoring procedures, potentially affecting clinical outcomes
While unremarkable to most, aspects of the EEG process can be upsetting to patients within certain demographics. The odour of medical-grade adhesives such as collodion, the noise of the air pump, skin irritation from electrodes, and manual handling of the patient’s head can cause significant discomfort, distress, and even pain in some.
Far from a superficial issue, this discomfort can have a negative effect on clinical outcomes. When patients feel like they’re being made to compromise on their quality of life for treatment, many will simply choose not to proceed, or to end the procedure, potentially delaying diagnosis and treatment that could improve their quality of life.
As such, prioritising patient experience during the study can improve patient compliance, supporting clinical outcomes and reducing the need for repeat monitoring.
Far from a superficial issue, discomfort associated with sensory input can negatively affect clinical outcomes for sensitive patients.
Who is affected?
Sensory issues are often (but not always) associated with neurodevelopmental disorders, head injury, or young age
Within the context of EEG, sensory issues normally manifest as an over-sensitivity to aspects of the connection and monitoring process. For affected patients, simple procedures like attaching electrodes or applying adhesives can cause distress, discomfort, or even pain.
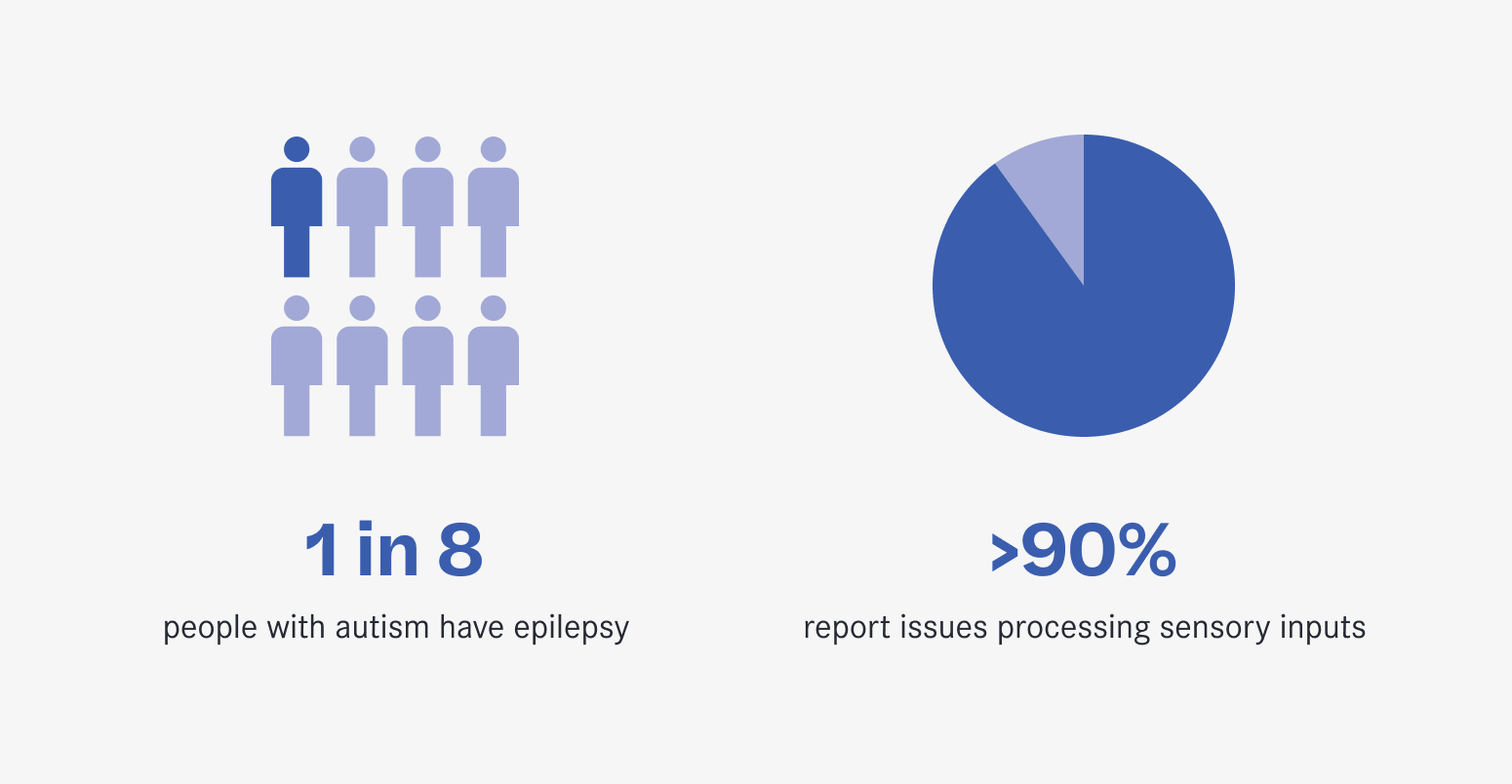
Neurodevelopmental disorders such as ADHD and autism frequently co-occur with sensory issues, with more than more than 90% of autistic people reporting issues processing sensory inputs. Coupled with high rates of comorbidity between autism and epilepsy – the latter affecting 1 in 8 autistic people – this demographic makes up a significant portion of those referred for monitoring.
Patients with a history of head injury or cranial surgery can experience scalp tenderness and sensitivity long after the event, making affixing electrodes potentially painful. Likewise, children may be distressed by repeated touching of their head or hair, especially by strangers.
Different patients can struggle with different aspects of the connection, and what may agitate one individual may be unremarkable to another. Understanding your patient’s individual triggers is essential to delivering a better monitoring experience.
Clinical scientists have a powerful role to play in supporting patients through the monitoring period, starting long before the connection appointment.
Setting patients up for success
Good patient experience starts well before the day of the connection appointment. Clear communication and careful preparation ahead of the study are key to patient comfort and success
Open and honest communication is always essential, but being patient-centric means tailoring that communication to the individual. For patients with sensory issues, that often means a more considered approach.
Some patients may struggle to understand printed materials, or will have specific questions outside the scope of a standard pamphlet. Following up written material with a phone call not only gives patients or their caregivers the chance to learn more about the study, but also helps to diffuse common anxieties around medical procedures by increasing familiarity with the procedure and the staff delivering it.
It also offers an opportunity for staff to get a better understanding of the patient’s needs, and apply that information at the connection. Offering a noise-sensitive patient earplugs, or knowing to choose a collodion alternative for a person who is sensitive to strong odours can make a huge difference to their overall experience, but only by talking to the patient will a clinical scientist know to prepare these accommodations.
Knowing the needs of your vulnerable patients allows for personalised accommodations during their appointment.
Delivering a comfortable experience
Small changes and accommodations during the connection process can improve patient comfort throughout the study, decreasing the chances of early disconnection
Minor environmental changes can significantly reduce the risk of sensory overload for patients with sensory issues. Small steps like dimming harsh lights, eliminating unnecessary background noise and limiting staff to only those necessary for the procedure can have a positive compounding effect on the patient’s mental state.
Uncertainty is a major cause of stress in patients of all backgrounds. Clinical scientists can minimise anxiety-inducing shocks by explaining each step of the connection process before and as they are taken. Warnings prior to touching the patient’s head, or that the glue about to be applied is cold, can allow patients to brace for the sensation, reducing its impact.
The most important accommodation clinical scientists can make is offering the time for breaks. A few minutes of deep breathing or focusing solely on a positive distraction can do wonders for a patient’s stress levels, allowing them to approach the rest of the appointment with confidence.
EEG is just one step in the diagnostic journey, but its central role in the diagnosis of seizure-like events makes it a crucial opportunity to positively affect patient experience.
Simple ways to support patients
The essence of patient-centric care is respecting a patient’s autonomy and individual needs, involving them in decisions and tailoring care accordingly
At Seer, we believe that every patient has the right to effective and compassionate care, delivered in a way that suits their individual needs. The techniques we’ve outlined are used in our Australian clinics every day, helping thousands of patients with sensory issues find the answers they need to guide their health without compromising on their comfort.
Key to that is our role as Australia’s largest provider of home video-EEG services. By taking EEG out of the hospital, we’re making diagnostics accessible to the millions of people around the world who struggle with inpatient monitoring, replacing uncertainty, discomfort, and inconvenience with familiarity, family, and ease.
If you’d like to learn more about our company or have any questions about our services, please visit our website or send your enquiries to home@seermedical.com
Refer to Seer Medical
Seer Medical has supported more than 10,000 patients through comfortable, reliable home-based monitoring. Learn how you can refer your own patients to us for a study.
Learn more
